欧博allbetStable Coronary Artery Disease (Chronic Co
Vasospastic Angina (Prinzmetal Variant Angina)
How to Cite This Chapter: Sibbald M, Pasierski T, Banasiak W, Leśniak W, Referowska M. Vasospastic Angina (Prinzmetal Variant Angina). McMaster Textbook of Internal Medicine. Kraków: Medycyna Praktyczna. https://empendium.com/mcmtextbook/chapter/B31.II.2.5.2. Accessed November 28, 2025.
Last Reviewed: March 29, 2025
Last Updated: July 17, 2019
Chapter Information
McMaster Textbook of Internal Medicine Editorial Offices
Editorial Office (Canada)
Section Editors: Matthew Sibbald
Authors: Matthew Sibbald
Editorial Office (Poland)
Section Editors: Andrzej Budaj, Wiktoria Leśniak
Authors: Tomasz Pasierski, Waldemar Banasiak, Wiktoria Leśniak, Maria Referowska
Past Contributors: Vikas Tandon
Main Documents Taken Into Account:
Writing Committee Members, Virani SS, Newby LK, et al. 2023 AHA/ACC/ACCP/ASPC/NLA/PCNA Guideline for the Management of Patients With Chronic Coronary Disease: A Report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2023;82(9):833-955. doi:10.1016/j.jacc.2023.04.003
Hokimoto S, Kaikita K, Yasuda S, et al. JCS/CVIT/JCC 2023 Guideline Focused Update on Diagnosis and Treatment of Vasospastic Angina (Coronary Spastic Angina) and Coronary Microvascular Dysfunction. Circ J. 2023;87(6):879-936. doi:10.1253/circj.CJ-22-0779
Ford TJ, Stanley B, Sidik N, et al. 1-Year Outcomes of Angina Management Guided by Invasive Coronary Function Testing (CorMicA). JACC Cardiovasc Interv. 2020;13(1):33-45. doi:10.1016/j.jcin.2019.11.001
Knuuti J, Wijns W, Saraste A, et al. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J. 2020;41(3):407-477. doi:10.1093/eurheartj/ehz425
Ford TJ, Stanley B, Good R, et al. Stratified Medical Therapy Using Invasive Coronary Function Testing in Angina: The CorMicA Trial. J Am Coll Cardiol. 2018;72(23 Pt A):2841-2855. doi:10.1016/j.jacc.2018.09.006
Definition and Clinical Features
Vasospastic angina (Prinzmetal variant angina) is a type of angina in which chest pain is caused by transient ischemia secondary to spontaneous macrovascular or microvascular coronary artery spasm. Chest pain generally occurs at rest and usually in the absence of flow-limiting coronary stenoses.
Symptoms include chest pain occurring at rest, commonly in the late night or early morning hours, which is frequently transient and lasts between 5 and 15 minutes (pain characteristics: see ). On occasion, it may also develop on exertion, although this is less common. Other associated symptoms may include nausea, diaphoresis, palpitations, dyspnea, and lightheadedness.
Diagnosis
Diagnosis is based on the occurrence of unprovoked chest pain at rest with accompanying ST-segment elevation (less commonly depression) on electrocardiography (ECG) (Figure 3.11-1) and absence of significant coronary artery stenosis on coronary angiography. If an episode occurs during coronary angiography, coronary spasm may be directly observed during the procedure. Intracoronary pharmacologic provocation testing with acetylcholine, ergonovine, or hyperventilation should be considered when the diagnosis is unclear.
In patients with recurrent pain Holter monitoring may reveal ST-segment changes with pain. Whether ST-segment elevation or ST-segment depression is seen depends on the severity of spasms: full occlusion causes ST-segment elevation, while a less severe spasm may cause ST-segment depression. Rises in the levels of biomarkers of ischemia depend on the duration of the spasm. While most times the spasm is transient, a prolonged spasm may lead to actual infarction and arrhythmia in up to 25% of patients.
Treatment
Medical Treatment
1. Modification of risk factors, particularly smoking cessation. Alcohol moderation/abstinence, particularly for those with alcohol-related flushing or known polymorphisms of aldehyde dehydrogenase 2 (ALDH2) associated with coronary vasospasm.
2. Low-dose acetylsalicylic acid (ASA).
3. Nitrates or nicorandil (or both).
4. High-dose oral calcium channel blockers: Diltiazem 120 to 360 mg/d, verapamil 240 to 480 mg/d (see Table 3.11-14). If treatment with 1 calcium channel blocker is not effective, add another calcium channel blocker of a different group or a long-acting nitrate (see Table 3.11-13).
5. Nonselective beta-blockers are contraindicated as they may exacerbate vasospasm.
Invasive Treatment
Percutaneous intervention is not recommended as the first-line therapy for patients with coronary vasospasm and nonobstructive coronary disease. Consideration may be given to percutaneous coronary intervention (PCI) if significant plaque (≥70%) is present and if the plaque is thought to be a trigger for localized vasospasm with the patient developing pain at rest. PCI of a vasospastic segment may be also of benefit in patients who are refractory to medical therapy if the vasospastic segment is clearly visualized on the diagnostic catheterization. Outcomes overall are variable, as vasospasm may occur in a different section of the artery, and thus medical therapy is considered the first-line treatment. Vasospasm-associated severe arrhythmias may require treatment with a pacemaker or implantable cardioverter-defibrillator (ICD).
Prognosis
Among patients with vasospastic angina, 95% survive 5 years from diagnosis. Prognosis is worse in patients with concurrent atherosclerotic plaque and in those with vasospasm-induced ventricular fibrillation.
Figures
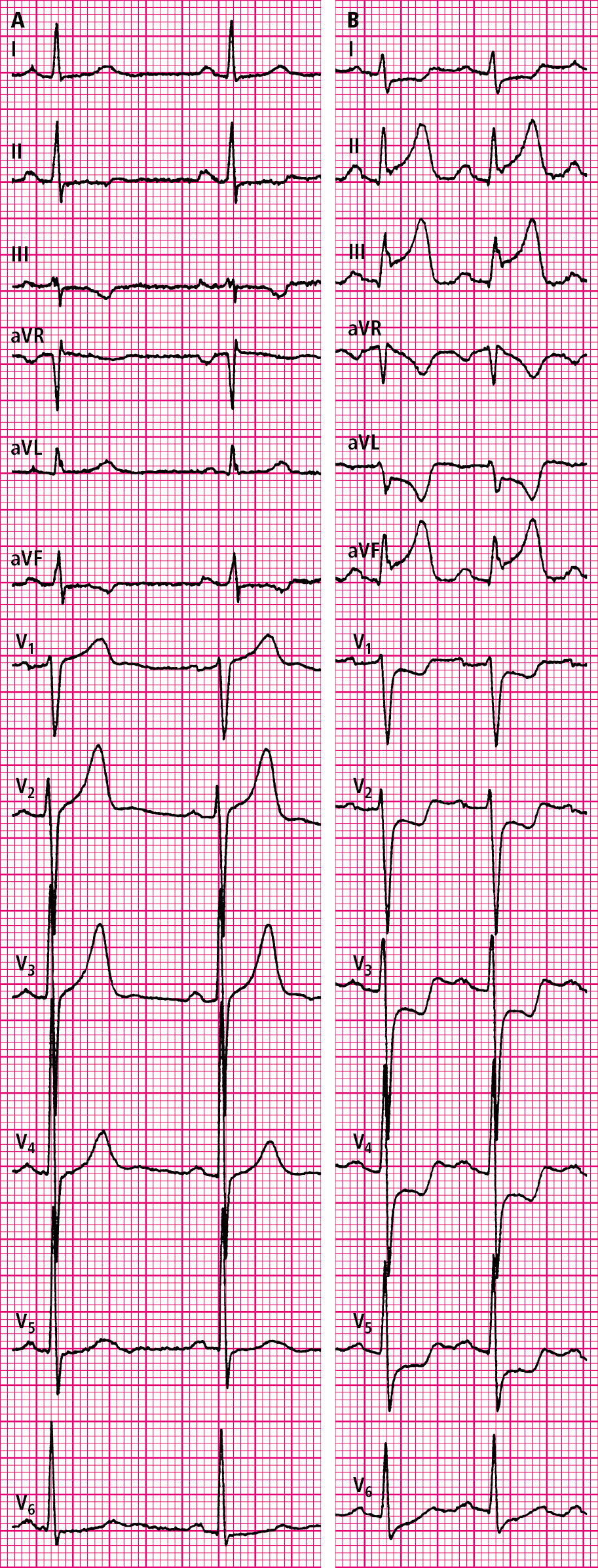
Figure 3.11-1. Electrocardiography (ECG) of a patient with vasospastic angina in a pain-free state (A) and during a pain episode (B). Figure courtesy of Dr Tomasz Pasierski.